Why does BPH happen?
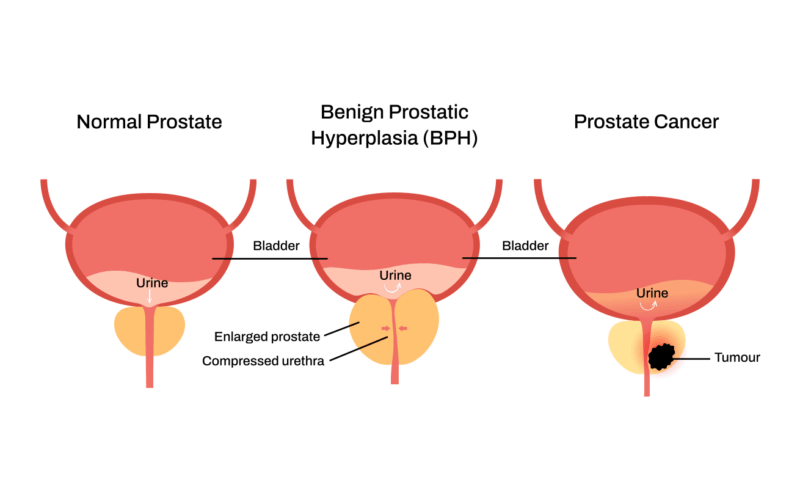
Benign Prostatic Hyperplasia (BPH) becomes more common as men age. The prostate is sensitive to lifelong hormonal changes, especially the balance between testosterone and dihydrotestosterone (DHT), which can stimulate prostate tissue to grow over time.
Genetics influence how strongly the prostate responds to these hormones — if close relatives had significant enlargement, the likelihood is higher. Weight and body fat can increase inflammation and shift hormone levels, which may speed up growth. Activity level also matters: regular exercise helps regulate hormones and reduce inflammation, while a sedentary lifestyle can contribute to earlier or more noticeable symptoms.
As the prostate enlarges, it can press against the urethra and bladder outlet, leading to symptoms such as slow flow, urgency, frequent nighttime urination, or difficulty starting. BPH is not cancer, but the symptoms can overlap, which is why evaluation is helpful when changes occur.
What actually causes prostate cancer?
There isn’t one single cause. Prostate cancer happens when normal prostate cells, for some reason, go a little “crazy” — dividing when they shouldn’t and growing in ways the body can’t regulate. These abnormal cells usually start in the outer portion of the prostate, where they can form tumors and, if not caught early, may spread beyond the gland. Age-related changes, genetics, and other biological factors all play a role, even though the full picture isn’t completely understood yet.
Age is the strongest factor. Prostate cells accumulate changes naturally as men get older. Most prostate cancers are diagnosed after age 55 simply because the prostate has had more time to develop these changes.
Family history matters. Having a father, brother, or close relative with prostate cancer increases your risk — not because cancer is “passed down” directly, but because certain genetic patterns can make prostate cells more likely to become cancerous over a lifetime.
Inflammation can contribute. Long-standing inflammation in the prostate — from infections, irritation, or chronic prostatitis — may play a role in cell changes over time.
Hormones also influence prostate cancer. Testosterone and dihydrotestosterone (DHT) help prostate tissue grow and function. Over decades, this hormonal environment can shape how prostate cells behave. However, current research shows that testosterone replacement therapy does not cause prostate cancer. It does not appear to increase the risk of developing cancer, but it can make an existing prostate cancer easier to detect by improving PSA accuracy.
Struggling with BPH symptoms?
Because the relationship between hormones and prostate cancer is complex, decisions around testosterone therapy should always be individualized and made on a case-by-case basis.
Even with these factors, many men still ask, “Why me?” The reality is that most men who develop prostate cancer have no obvious cause — no major risk factors, no lifestyle triggers, no clear explanation. It’s a common condition that often develops quietly over many years.
Because early prostate cancer almost always causes no symptoms, screening and monitoring PSA levels remain the best way to detect it early, when treatment options are broad and outcomes are strongest.
Does diet really make a difference?
Diet can influence overall prostate health — much like it affects the rest of your body and other organs. Research consistently shows that diets rich in vegetables, fruits, lean proteins, and healthy fats are linked to better long-term health outcomes.
For prostate health specifically, a protective diet generally limits processed meats, excessive dairy intake, and diets high in saturated fats. Many men also choose to reduce their intake of highly processed seed oils (such as soybean, corn, or canola oils) in favour of more natural fat sources like olive oil, nuts, avocados, and fish. These foods support a healthier metabolic and inflammatory environment.
Diet isn’t a cure for prostate conditions, but it’s an important part of a healthy approach and can complement monitoring, lifestyle changes, and medical treatment when needed.
What should I know about PSA?
PSA (Prostate-Specific Antigen) is a protein made by prostate tissue. Levels can rise for many reasons — BPH, inflammation, infection, recent ejaculation, cycling, medical procedures, or cancer. A single PSA number doesn’t provide the full picture, but does raise our suspicion. Watching how your PSA rises or stays stable over time gives important context, especially since PSA naturally increases with age and prostate size. That pattern helps us determine whether your result is significant and needs follow-up.
A rising PSA should be evaluated, even if the value is still “within normal range,” because early prostate cancer often has no symptoms. An MRI or further testing can help clarify whether the rise is due to benign causes or something that needs attention.
How fast should I act if my PSA is rising?
A rising PSA doesn’t always mean cancer — many benign factors can cause temporary increases. But a change in PSA should be evaluated, especially if the rise continues over time. Because wait times for urologist appointments and biopsies can be long in Canada, many men choose to arrange a timely assessment with our team. This may include MRI and/or biopsy, if appropriate, and helps clarify whether the rise is due to a benign cause or something that needs attention.
A PSA increase of more than 20% a year is the general rule of thumb that would prompt further investigation.
What does “localized”, “advanced” and “metastatic” mean in prostate cancer?
Localized prostate cancer means the cancer is contained within the prostate gland, with no evidence of spread through the capsule or to lymph nodes, bones, or other organs.
Many localized cancers are multifocal (more than one area within the prostate), which is common. Treatment options depend on the size, grade, number of lesions, and where they are located — not simply on whether the disease is inside the gland.
Advanced prostate cancer means the pathologic features are more aggressive — such as a higher Gleason score or a larger volume of cancer. These factors may make someone ineligible for focal treatment; however, whole-gland ablation with HIFU may still be an option in some cases.
Metastatic prostate cancer means the cancer has spread beyond the prostate. This can include the seminal vesicles, lymph nodes, bones, or surrounding tissues. Metastatic cancers require broader, systemic treatment approaches.
What if my MRI or biopsy results don’t match — or different doctors disagree?
It’s not unusual for imaging reports to differ slightly, especially when the findings are subtle. Sometimes one radiologist may describe an area as more suspicious while another may see it as low concern — both are using the same information but their interpretations can vary.
This doesn’t mean something is wrong. It simply means the picture isn’t completely clear yet. In situations like this, your specialist may recommend repeating the MRI or doing a targeted MRI Fusion biopsy to get a more precise diagnosis. These steps help ensure you get the most accurate assessment before making any decisions.