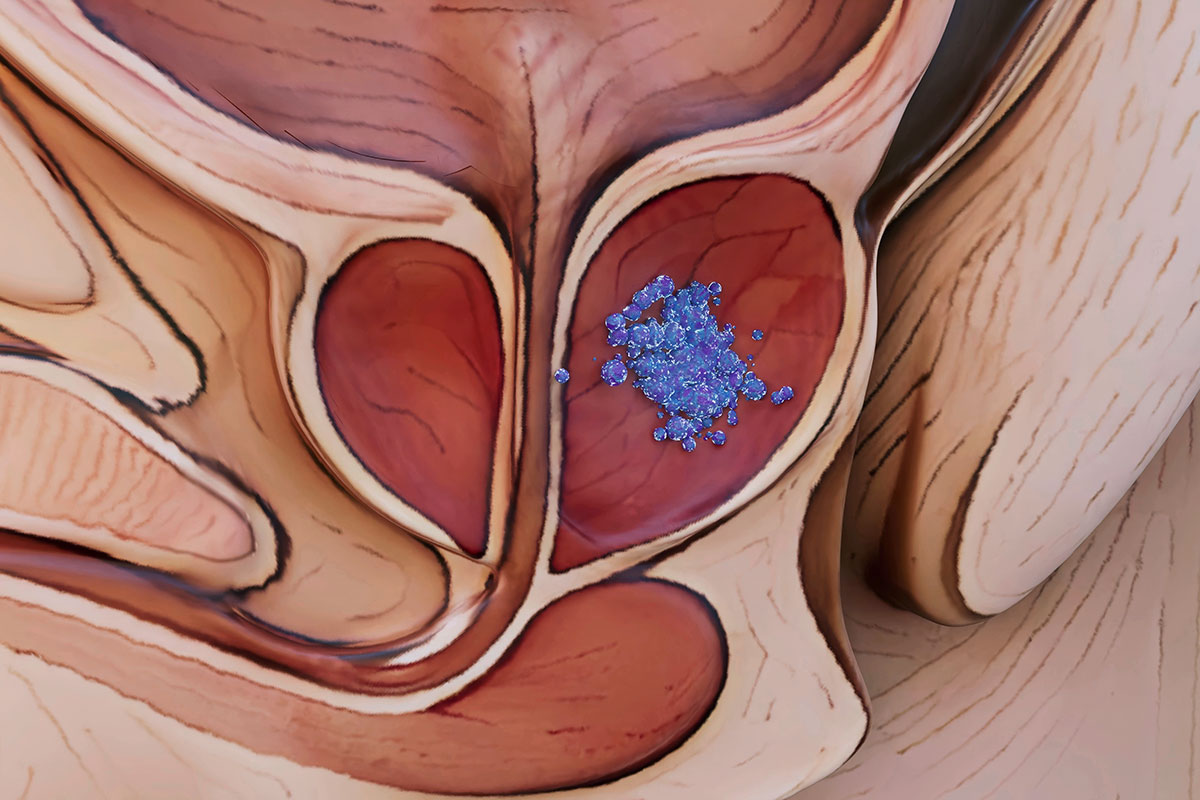
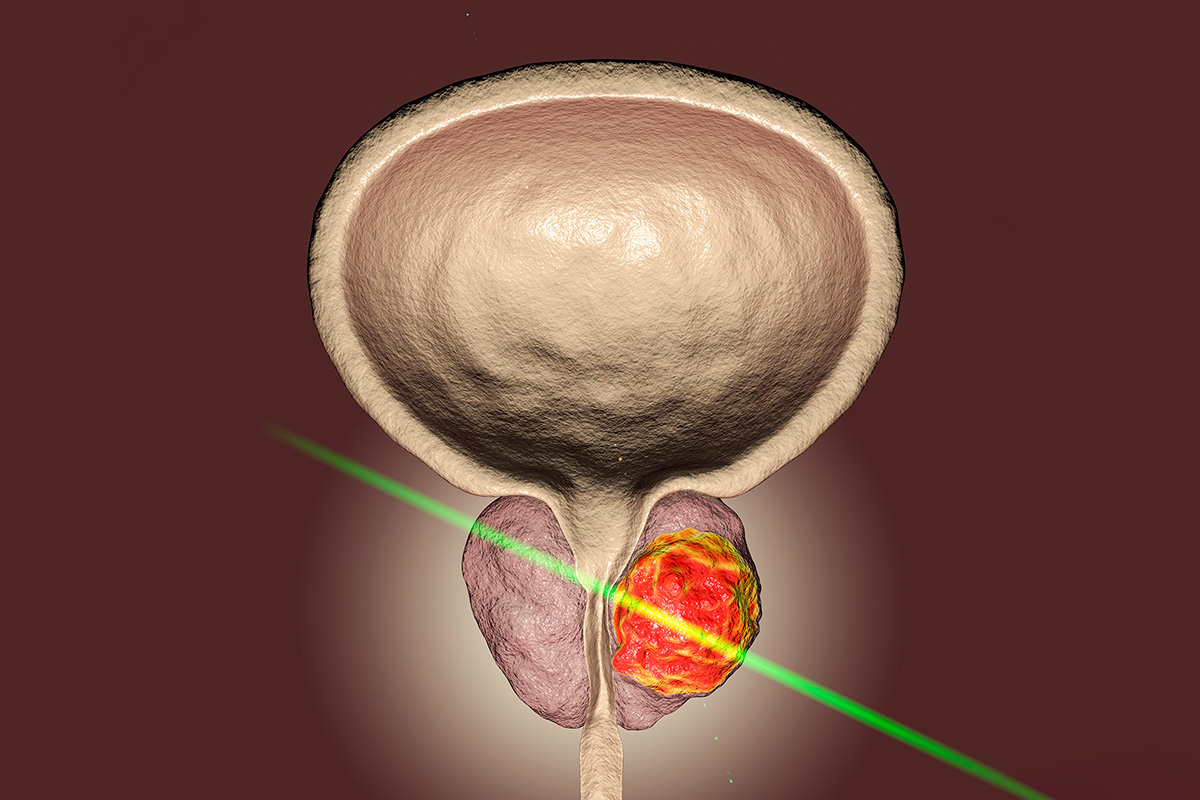
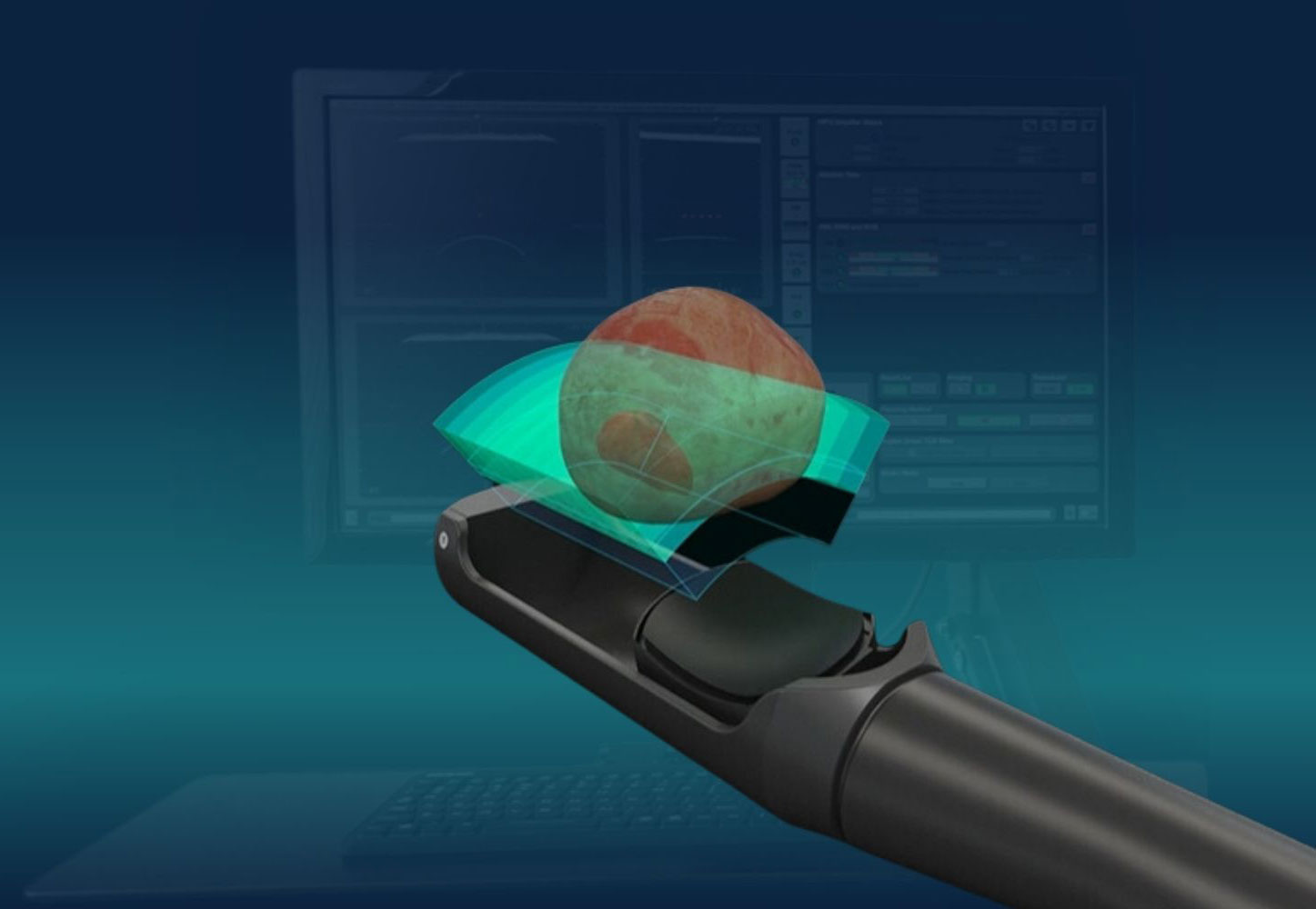
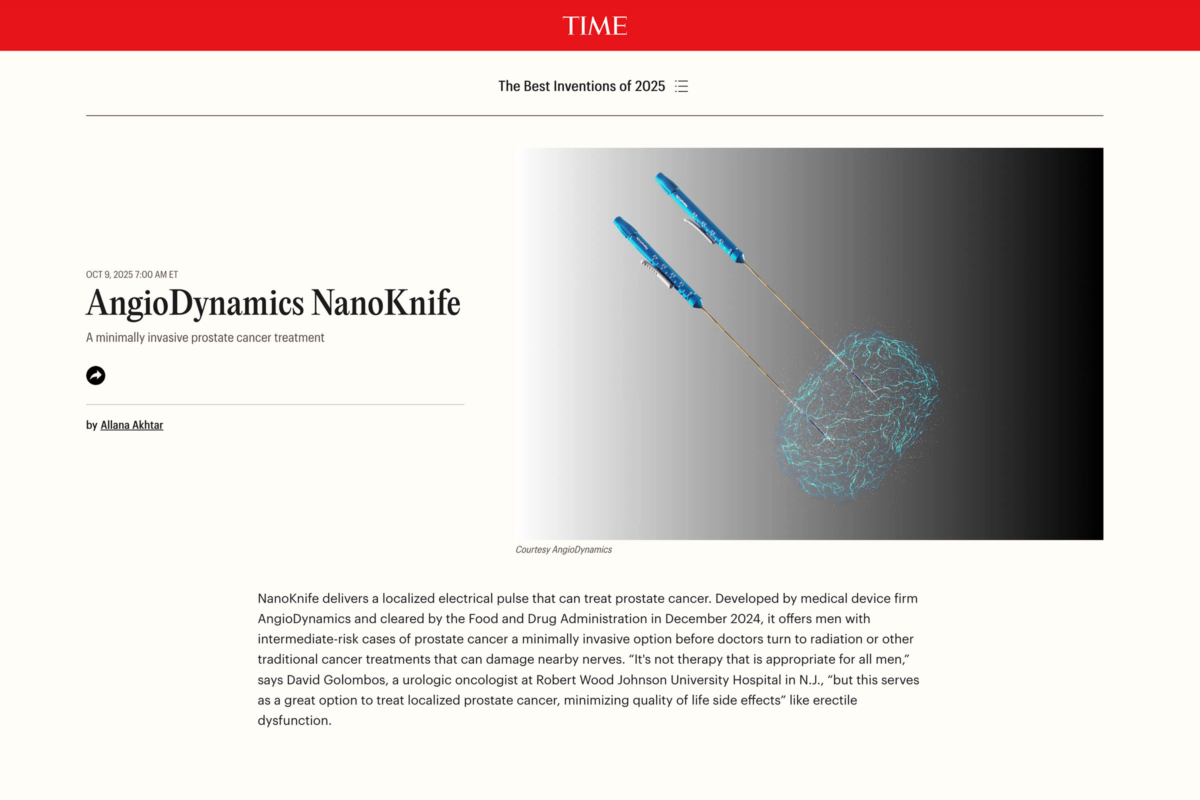
Urology Innovations Canada (UIC) is a leading provider of advanced, minimally invasive treatments for prostate cancer, BPH, and other urological conditions. As the first clinic in downtown Toronto to offer NanoKnife (IRE) and one of the most experienced HIFU providers in North America, we specialize in precision focal therapies that prioritize effectiveness while preserving quality of life. Our expert team serves patients from Toronto, the Greater Toronto Area, across Canada, and internationally.
The reviews and testimonials featured on this website represent the individual experiences of our patients. Results may vary from person to person, and no outcome is guaranteed. These reviews are intended to provide insight into the experiences of others and should not be used as a substitute for professional medical advice. Please book a consultation with one of our Toronto urologists to determine the best course of treatment for your unique needs.